1: Only about 15% of the CO2 generated from cellular respiration is expelled when one is at rest and breathing normally. CO2 plays a critical role throughout the body.
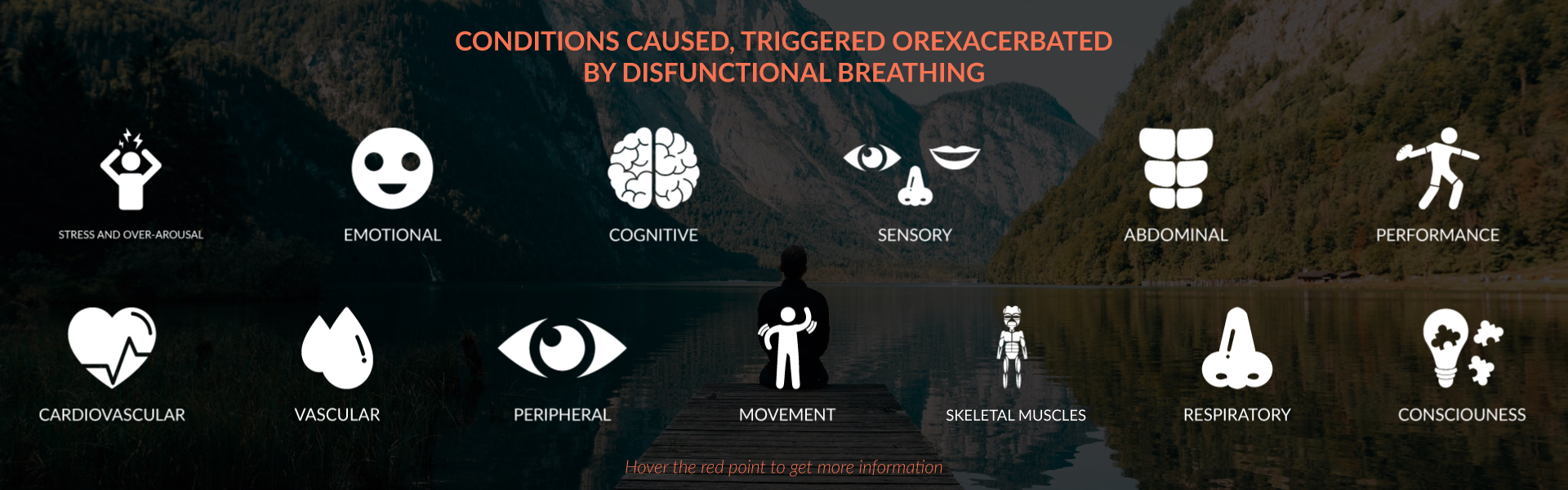
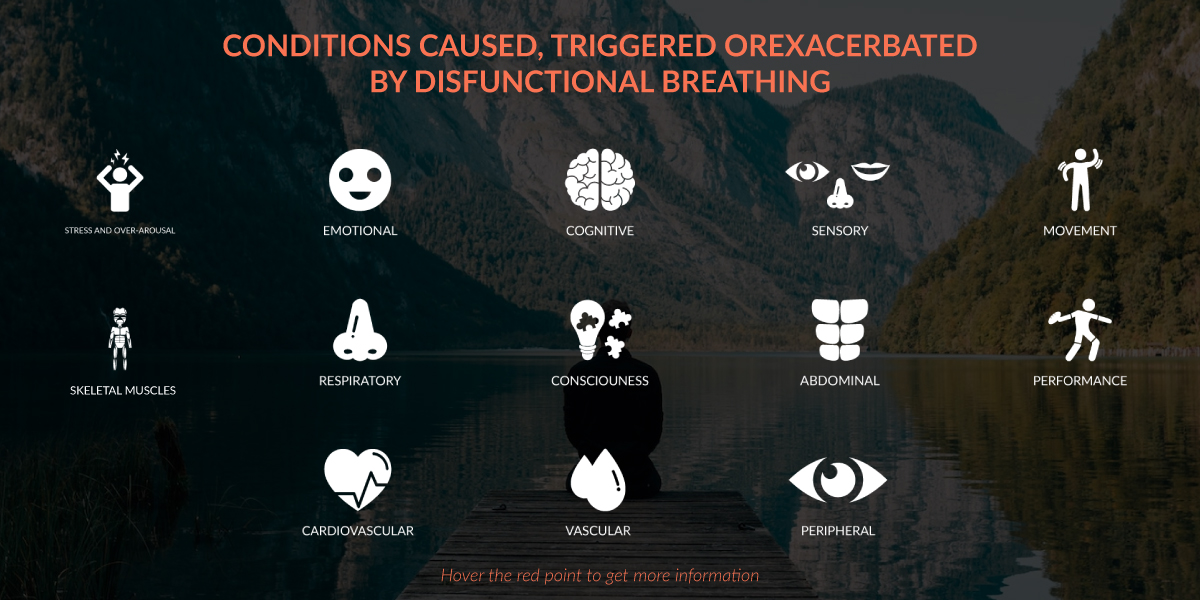
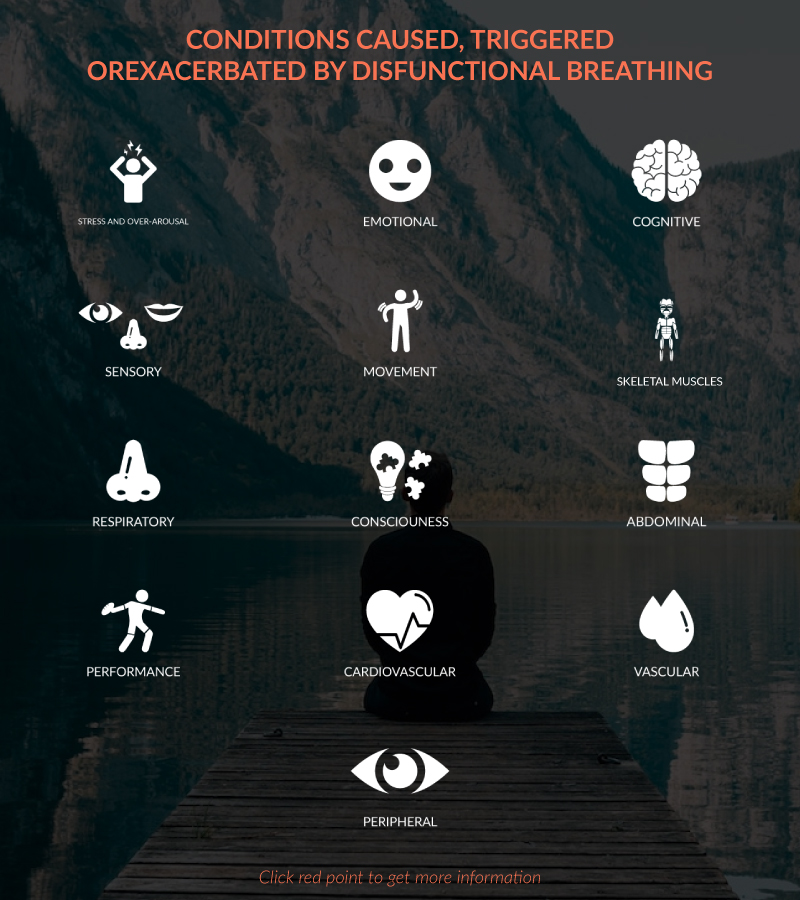
When not in adequate supply, internal chemistry goes awry and “lights start to flicker” in the body. The variety of symptoms that can show up (see figure 1) are a function of genes and other epigenetic variables going on in one’s life. Unfortunately, very few clinicians or practitioners realize that these symptoms are triggered, exacerbated or caused by internal chemical imbalances associated with dysfunctional breathing.