Hypocapnia is a condition defined by the arterial partial pressure of CO2 being below 35mmHG which in turn causes blood plasma pH to rise above 7.45… resulting in respiratory alkalosis… pH that is too high! Hypocapnia that is a function of dysfunctional breathing (breathing too deep or too fast to offset metabolic requirements) is known as behavioural hypocapnia.
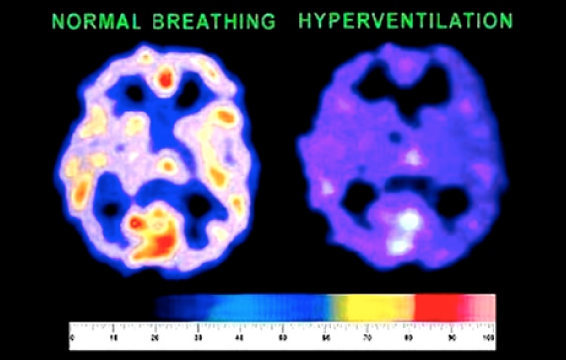
Behavioural hypocapnia is a condition where the partial pressure of arterial blood CO2 levels (PaCO2) falls below 35mmHg from over-breathing. This, in turn, pushes pH of interstitial fluids beyond their thresholds as per the Henderson-Hasselbach equation listed above. Behavioural hypocapnia is often learned and reinforced subconsciously, so can be difficult to undo without professional assistance and the discovery process of personal reinforcements that will unknowingly keep a dysfunctional breathing habit in place. Consequences of long-term hypocapnia (symptoms) are again outlined in figure 1.1. The figure below shows a fMRI of a brain that has less blood-flow due to vasoconstriction… one result of over-breathing. For every 1mm Hg below 40mmHg of CO2 partial pressure, the average blood flow reduction is 2%. Many people who overbreadth have CO2 levels down at 25 – 35mmHG… an oxygen/blood flow reduction of 20% to 30%!